Poster presented at ASM Microbe 2017: Session 035, Friday Poster 038. Title: Comparative Evaluation of New Respiratory Quinolone DC-159a or Moxifloxacin Containing Regimens in a Murine TB Model. H. Nakamura, Y. Horita, N. Doi; Japan Anti-Tuberculosis Association, Res. Inst. of Tuberculosis, Tokyo, Japan
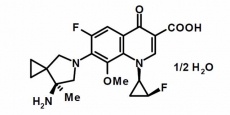
Abstract: Background: For the assessment of the potential in vivo efficacy of new generation respiratory quinolone DC-159a (D, Daiichi Sankyo Co., Ltd) to shorten the total treatment duration for TB, we conducted a comparative study of Pretomanid (PA-824: P) containing combination regimen PDZ (P: PA-824, D: DC-159a, Z: Pyrazinamide) with Moxifloxacin (M) containing combination regimen PMZ, and current standard regimen RHZ (R: rifampicin, H: isoniazid) using murine TB model. Relapse ratio of each treatment group was also investigated. Methods: Female BALB/c mice (Japan Charles River) were infected with Mycobacterium tuberculosis H37Rv (logCFU=6.04/mouse) via intratracheal route, and treatment was started from Week Four post infection. Treatment groups were: 2PDZ/2PD, 2PMZ/2PM, and 2RHZ/4RH. Dose sizes were: D 50 or 100, M 50, 100 or 200, P 20, R 10, H 10, Z 150 (mg/kg-mouse). Drug cocktail was administered 200 µl/mouse/day, 5 days/week, for 4- or 6-months. Relapse ratio in lung and spleen of the each treatment group (n=10~12/group) was investigated four months after completion of chemotherapy. Results: (1) Lung: PD100Z>PD50Z=RHZ=PM200Z>>PM100Z >PM50Z. PD100Z, PD50Z, RHZ and PM200Z groups negative converted number of CFU after 14-, 16-week treatment, respectively. (2) Spleen: PD100Z>RHZ=PD50Z>PM200Z>PM100Z>>PM50Z. PD100Z, RHZ, PD50Z, PM200Z and PM100Z groups negative converted number of CFU after 8-, 10-, 12- or 16-week treatment, respectively.
However, PM50Z group could not negative convert number of CFU in Spleen; recorded final logCFU 1.1. (3) Relapse rate (%): Lung: RHZ: 7.1, PD100Z: 60, PM200Z: 90, PD50Z: 100, PM100Z: 100 and PM50Z: 100% (n=10~14/each group). Spleen: RHZ: 0, PD100Z: 30, PM200Z: 90, PD50Z: 100, PM100Z: 100 and PM50Z: 100% (n=10~14/each group). Conclusions: (1) DC-159a (100mg/kg) combination regimen showed the best efficacy than any other combination groups. (2) DC-159a containing regimens were superior to those of Moxifloxacin containing regimens. (3) DC-159a would shorten the total treatment duration for TB.
2016: DC-159a showed the highest activity against drug-susceptible (DS) TB, quinolone-resistant (QR) MDR-TB and NTM isolates than those of MFLX, GFLX, LVFX and RFP. Activity of DC-159a against QR MDR-TB (MIC90: 0.50 µg/ml) was comparable to that of LVFX against DS-TB isolates. The highest anti-TB activity including MDR strains due to potent inhibitory activity against wild-type and altered DNA gyrase of M. tuberculosis. In the QR MDR-M. tuberculosis infection model, DC-159a treatment groups recorded notable “mean survival days†more than 2~3 times superior to MFLX, LVFX, INH and RFP. In the Drug-Susceptible-M. tuberculosis infection model, DC-159a treatment groups exhibited the best “EBA†and the highest “Log Reduction of CFU in Lungsâ€, which was superior to those of MFLX, LVFX, INH and RFP. Favorable PK ADME profile, high AUC, Cmax, and target distribution. Superior in vivo efficacy of DC-159a in murine TB models might be attributed to its rapid uptake and high concentrations in lungs.